
| Library |  |
|
 Earth Air Fire and Water
Earth Air Fire and Water
The Pharmageddon Herbal
Compounding
Ivor Hughes
Chapter 11B Continues.
Methodology for Lotions and Creams 11.21
By definition, lotions and creams
are emulsions. Lotions
are oil in water (O/W) The Creams
are water in oil (W/O). It is necessary to study the
formula to decide which type of emulsion it is. Because each type needs to be
mixed (homogenised) by a different methods to prevent cracking or creaming.
Calculate the oils, fats and waxes as a percentage of the total formula. Then calculate as a percentage, the total of the water, and water soluble constituents. If the oil phase is the greater, then the more viscous the product, and will tend to be a cream. If the water phase is the greater, then the product will tend to be a lotion.
O/W preparations may be homogenised by an egg whisk or an electric mixer. W/O preparations will need to be slowly stirred, either by hand or by a paddle mixer set a slow speed. The reason is that, if air bubbles are introduced during the mixing process, then the preparation may crack or cream.
The following formula is an O/W moisturising cream. It is a variation on an ancient formula, originally attributed to Galen. It is found in many of the older pharmacopoeias under the name of Galens Cerate. Borax was the usual emulsifying agent specified. Borax is toxic and damaging to the skin. In the formula below, mucilage of Quince seed is the emulsifying agent
| Bees Wax | 115g |
| Palm Kernel Oil | 110g |
| Oil of Almond | 550g |
| Mucilage of Quince | 20g |
| Distilled Water | 195g |
| Gum Benzoin Extract | 10ml |
| Essential oil of Rose | 1.0ml |
Understand that the above formula will need to be adjusted because of the provenance of your materials. Prepare a water bath and add the first three ingredients. Grate the bees wax into small pieces and add them to the oil phase. Stir until all of the oil phase is in a homogenised state.
Add the mucilage to the distilled water and mix. Take the temperature of the oil and heat the distilled water to the same temperature. Then stirring steadily, slowly add the water phase to the oil phase.
Remove from the heat, and add the Benzoin extract and oil of rose. Then beat or mix vigorously until cool.
The above formula is an Emollient, and may be suitably medicated or lightly perfumed, according to its end use. As a general rule of thumb, add the waxes to the oil. A word of warning, never heat the oil phase over direct heat and then add water. This will cause the hot oil to erupt with possible dire consequences. Always use a water bath or double boiler.
The methodology described may be considered as standard. . If compounding from a Pharmacopeia or Dispensatory, any deviations or special requirements will be clearly stated.
The Ointments (Unguentum) 11.22
The ointments, as a class of
medicament, have a long and venerable history. As a compound, the ointment is
ingenious, and may be made to serve many different purposes.
1. As an emollient to soften or soothe the skin.
2. As a protective barrier for the skin against noxious substances, insects or ultra violet rays.
3. As a vehicle for medicinal substances which are to be;
A. An application to the skin for antiseptic or anaesthetic purposes.
B. Absorbed through the skin for introduction of the medicament to the circulation.
Ointment bases are also used
for suppositories and pessaries,
for rectal or vaginal administration of a medicament. When beeswax is specified
in a formula for medicinal purposes, it should be taken to mean yellow
unbleached wax. (Cera Flava), and not the bleached wax (Cera Alba) .White
wax finds use in cosmetics purely because it presents a better appearance.
Experience has demonstrated that preparations made with yellow, unbleached wax has better keeping qualities. No doubt because it has not been chemically altered.
The ointments are of great variety and serve as a vehicle for hundreds of different substances. The ointments in turn, are made from a wide variety of base materials which may be ;
(A) Animal fats. (B) Insect exudations. (C) Vegetable exudations. (D) Mineral oils and wax. (E) Synthetics.
Substances which fall under the head of A, D and E, should as a general rule, be avoided, because there is the possibility of the uptake of undesirable substances, and in the case of the Animal fats, there are also some unresolved questions relating to hormones and the allopathic antibiotics.
When compounding an ointment from published formulae, then substitutions for undesirable substances may need to be made. Accordingly, the purpose of the ointment must be considered, i.e., is the ointment, a barrier, an emollient, or is it to introduce medicaments to the circulation?. In addition, consideration must be given to climatic temperatures, Tropical, Temperate or Cold. Therefore, the two factors are Absorbency and Melting Point, of the selected substance.
| Vehicle | Melting Point | Absorbency |
| Beeswax (Cera flava) | 57 to 64C | Minimal |
| Coconut or Palm oil | 25 to 29C | Readily |
| Vegetable Oils | ................ | Readily |
| Paraffin Wax | 50 to 60C | Minimal |
| Lanolin (Wool fat) | 40 to 41C | Readily with oil |
| Petrolatum | 40 to 46C | Minimal |
| Purified Lard | 36 to 40C | Readily |
| Purified Suet | 44 to 45C | Readily |
| Theobroma (Coco butter) | 30 to 35C | Readily |
Methodology of Preparation 11.23
Prepare a water bath.
If the compound calls for a fixed oil, then add the
oil first and melt the other ingredients
in it. If the formula is comprised of waxes and fats,
then add the substance with the
highest melting point first,
and then melt the other substances in it. Remove from the heat, then stir or use
an electric mixer until the ointment has cooled.
Adding the Medicament 11.24
The incorporation of ground plant material
to an ointment base, is sloppy practice and leads to many uncertainties, e.g.
the degree of extraction
obtained by the ointment base materials is an unknown,
therefore, it presents a problem of posology. Secondly, unless a paint or shear
mill is used in the incorporation process, then a grittiness is bound to occur.
The medicament is most easily prepared from a 1 : 1 Extract, by evaporation over a water bath, or by distillation under reduced pressure. It should be reduced to a soft or pasty extract for incorporation into the ointment base. Gently heat the base until it is easily worked, but not in a molten state. The temperature should not exceed 30C. The medicament may then be incorporated into the ointment. At this stage, unless there is a problem of compatibility, a suitable inhibitor should also be added. It must be thoroughly mixed until an even dispersion has been achieved. Allow the finished ointment to congeal. It is then ready for use. To pour it into jars to set warm the ointment until it is pourable. Seal the jar with an airtight lid and allow to solidify.
Ointment Posology 11.25
The degree of absorption of a
medicament from an ointment base, cannot be known with any certainty,
because of the variables involved, e.g. the strength of the extract, the skin
type involved, individual idiosyncrasy and the absorbency of the base.
Therefore, the medicament must not exceed 10% of the total product, i.e., 1 :10.
We arrive at the correct amount of soft extract to use by the
following method;
Firstly, calculate the mass of the total finished ointment, then convert the mass to volume. Then calculate 10% of that figure, which is the amount in millilitres of a 1 : 1 extract, that must be added to the ointment base.
Reduce the liquid to a soft extract, and then incorporate it into the ointment. There will be exceptions, for example, strongly irritant substances such as extract of Capsicum, in which case the soft extract must be prepared in the same manner as a homoeopathic ointment, i.e., from a Mother Tincture of 1 :10. If following the instructions from a Pharmacopeia or Dispensatory, the quantities will be stated.
Useful Formulae 11.26
The following formulae will be
found useful for a variety of purposes. If a preparation is to contain large
amounts of liquid or water, then those formulae that contain Lanolin will absorb
the liquid in a satisfactory manner. When preparing an ointment, the compounder
is urged to ensure that the base will meet the criteria required. This is simply
achieved by testing the ointment on themselves. If the ointment is too stiff,
then it may be rectified by the addition of more oil, or a substance which is of
a lower melting point than that of the beeswax. If it is too soft, then the
addition of a substance of higher melting point will stiffen the product.
| Simplex | Basic | Barrier | Soft |
| Beeswax......1 | Beeswax......1 | Theobroma..1 | Beeswax......1 |
| Oil................1 | Lanolin........1 | Beeswax.......1 | Lanolin........1 |
| ...................... | Oil................1 | Oil.................2.5 | Palm Oil......6 |
Pessaries, Suppositories and Bougies. 11.27
Pessaries and Suppositories
are designed for insertion into the rectal and vaginal orifices of the human
body. For practical purposes,
there is no difference between the two.
However, by convention,
Pessaries are for vaginal
insertion and the Suppositories are for rectal insertion. The purpose is
to introduce medicaments to the mucous membrane of the orifice.
As a vehicle for the medicament, it is essential that the melting point should not exceed 37 Centigrade. Nor yet so low that it would melt at lower temperatures. Theobroma is the substance that meets the criteria. For children, the weight of the vehicle should not exceed 1g and for adults, 4g.
The bougie is designed for nasal insertion. There is no reason why such products may not be suitably medicated for insertion in a cleaned ear.
The
pessaries, suppositories and bougies
are formed in moulds. These may be conveniently made from tin foil or
alternatively, from polythene syringes from which the nozzle has been cut. The
method of preparation is the same as that of the ointments.
The product may be poured into the moulds in a molten state, or they may be formed by hand when the substance is in a suitably plastic state.
Salve Sticks 11.28
Salve sticks are almost identical to the suppositories in shape and base
composition. They are designed for the topical placements of medication to a
specific area of the skin. In the same way that lipstick is applied. The
following formulae for a cold sore salve will outline the principle.
| Propolis Salve | Melissa Salve |
| Almond Oil ........................ 30ml | Almond Oil ........................ 30ml |
| Beeswax...............................30gm | Beeswax...............................30gm |
| Theobroma...........................30gm | Theobroma...........................30gm |
| Propolis Tincture (1.4) .......10ml | Oil of Melissa ........................1ml |
Capsules, Pills and Tablets. 11.29
A most convenient form
of oral administration of a medicament, is by the use of tinctures or liquid
extracts. However, there are occasions when that form is contra-indicated. In
which case, a capsule, pill or tablet would be the choice of vehicle.. The
incorporation of a powdered crude drug into a carrier substance, is bad practice
and should be avoided.
Capsules may also be used as suppositories or pessaries. The end of the capsule may be removed with a sharp blade or alternatively pierced with a needle to facilitate the release of the medicament. The excipients and mass used must be hydrophilic (water loving), in order to enhance the bio availability of the medicament.
Capsules; The medicament may be in granular or soft extract form, which is enclosed in a 2 part capsule, made either from vegetable gel or keratin (gelatine). Given the current problems that are surfacing over the use of cattle by products.. It must be remembered that, there are no specific tests for BSE whilst it is in the incubation period, therefore, it would be wise and ethical to avoid the use of gelatine capsules.
The specifications for some common capsules are as follows;
Table 11.29A
|
Specification |
Size 0l |
Size 0 |
Size 1 |
Size 2 |
Size 3 |
Size 4 |
|
Joined length in mm |
24.44 |
21.93 |
19.61 |
18.03 |
15.95 |
14.56 |
|
Empty weight mg |
112 |
100 |
78 |
62 |
51 |
41 |
|
Capsule capacity cc |
0.835 |
0.750 |
0.540 |
0.420 |
0.310 |
0.250 |
N.B. Tolerance limit for weight is
� 10 %. Tolerance limit for length
is � 03 mm.
Capsules should disintegrate in not
more than 8 minutes in a solution
of 0.5% w/w HCI, at 36� to 38�
C.
The pH should be between 5 and 7.
Enteric Coated Capsules 11.30
Enteric coatings are used to delay or prevent
the release of a medicament until it reaches the duodenum.
The stomach environment is acid and the duodenum alkaline.
Suitable materials that will dissolve over an alkaline gradient are the natural waxes,
either vegetable or insect, e.g. beeswax. Shellac is also widely used. Shellac (lac)
is a resinous substance produced by a scale insect, which encrusts the twigs of
trees, upon whose sap it feeds. The coating may be prepared from 2 parts
of the resin and one part of warmed alcohol 90%.
Coating the Capsules 11.31
When coating capsules by hand there are 2 methods in general use:
1. By Rotation - This method is most suitable for wax coatings. Warm a glass flask or beaker in a water bath and add a small quantity of wax. When it has melted remove the flask or beaker from the water bath, add some capsules and gently rotate the flask by hand until an even coating has been applied. The rotation of the flask or beaker will prevent the capsules from sticking or clumping. Continue to rotate the flask until the wax has all solidified. Be sure to check for compatibilities when choosing a wax..
2. By Spraying - This is the preferred method for shellac coatings. A suitable sprayer may be purchased from a hobbyists model shop. Drying of the coating may be achieved by the judicious use of a hair dryer applied at a distance. Warm the shellac over a water bath. Introduce it to the sprayer. Place the capsules on a stainless steel mesh in a well ventilated place. Spray and dry. Extra coatings may be employed if required.
Pills and Pill Mass 11.32
The use of pills in
conventional pharmacy practice has been replaced by the capsule or tablet.
Nonetheless, they lend themselves to herbal compounding and are most conveniently made.
The pill is in 3 parts.
1. The medicament
which may be either liquid, soft or dry.
2. The mass or bulking agent. This should be an emollient substance which will not interact with the medicament. For example: powdered Marshmallow Root, Liquorice Root or a starch such as Arrowroot or rice flour. Wheat or Cornflour should be avoided, in case of gluten allergies.
3. The excipient or binding agent. If the medicament is in the form of a liquid or soft extract, then that in itself will be sufficient to form the pill mass. Suitable excipients are, distilled water, ethanol, syrups, honey, or mucilage of acacia.
A lubricant will be needed, which is usually the powdered Talc specified by a pharmacopeia. This is natural magnesium silicate which has been suitably purified and is neutral to litmus. The lubricant prevents the mass from sticking to the die. The talc is used to dust the die and punch.
The whole must be thoroughly mixed and sheared in a suitable mortar (levigated) to ensure an even dispersion of the medicament throughout the mass. When the mass is in a suitable state it may be pressed into moulds. The mass is pushed into the mould by use of a spatula.
A suitable mould
may be made from a stainless steel bar (The die),
in which appropriate size holes are drilled. The pills may then be ejected by a
rod (The punch) that matches the die. The pills may then be lightly
dusted and either left as they are, or formed into a sphere by lightly rolling
it in a circular motion, either between the gloved hands or between a concave
and convex surface.
Tablets ( Tabellae )
11.33
Tablets are of two types.
1.
A dry compressed substance.
2. A dry moulded substance.
Both of which serve the same function as a Pill.
Moulded Tablets 11.34
Moulded tablets are prepared
from a medicament and an
extender, such as lactose
or dextrose powder. If the medicament is a liquid or a soft extract, then
the ingredients should be placed in a mortar and thoroughly triturated with
sufficient extender to render the whole into a stiff paste.
If the medicament is in dried form, it must be powdered and thoroughly triturated with the chosen extender. Then sufficient Alcohol (60%) is added to produce a stiff pliable mass. The mass is pushed into the holes of a die of suitable size with a spatula. They are then removed with the punch and allowed to dry at room temperature.
Ideally, a non coated tablet should be thoroughly dissolved within 15 minutes of ingestion. If the tablets are coated with a substance to hide the taste, then they should dissolve within a maximum of 1 hour. If the tablet is enteric coated, that does not apply.
Moulded tablets are less time consuming to prepare. However, there are problems with disintegration times. As a general rule, the method should be reserved for pastilles or troches, which will be covered later in the text.
Compressed Tablets 11.35
There are two methods
of preparation which are suitable for the manufacture of compressed tablets;
they are;
1. Dry Granulation.
2.
Moist Granulation.
If using the dry method, the medicinal extract must be in granulated form. Lightly dust the granules with purified talc for lubricant purposes, and pass the granules through a number 16 mesh sieve.
If there is an insufficiency of granules to form a tablet, then an extender or mass may be used. The mass should not exceed 10% of the total weight. Load the die with the ingredients. Place the punch in each hole in turn and give a smart tap with a mallet. The tablet is then formed. The compressed tablets are then ejected with the punch.
The moist method may employ either granules or a soft extract. If granules are to be used, then add to them the mass and the excipient. The whole is then thoroughly levigated to produce a barely cohesive mass.
The excipient should be 60% alcohol, which will evaporate readily. Care must be taken to ensure that the mass is barely moistened, and that it will pass through a 16 mesh sieve without sticking. The resulting granules may then be dried at a temperature not exceeding 60 centigrade. Lightly dust the granules with talc by rotating them in a flask or a beaker. The excess talc is removed by sieving. The granules are then ready for compression If a soft extract is used instead of scales or granules, then the excipient should be omitted.
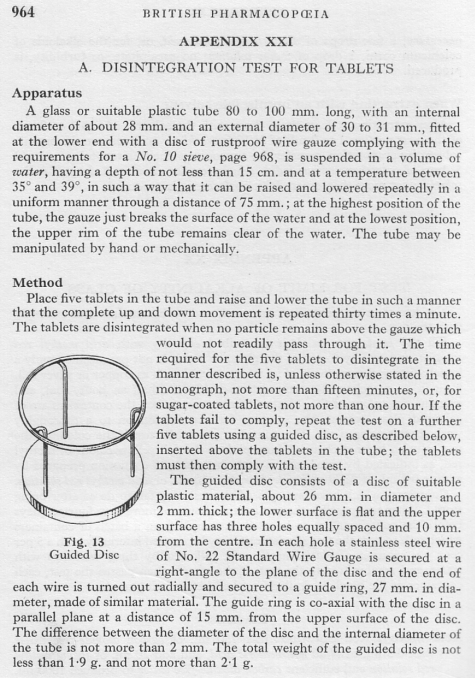
Tablet Disintegration Test 11.36
Extemporaneous preparations,
that is, those for which no formula is used, will of necessity, undergo a
disintegration test to ensure that the tablets dissolve in the correct portion
of the digestive tract. The following simple test is extracted from the British
Pharmacopoeia 1958.
Figure
11.36A
Lozenges
or Troches 11.37 The purpose is to deliver analgesic, anti-bacterial, astringent or demulcent substances, to the mucous membrane of the mouth or throat. They are formulated to slowly dissolve in the mouth by salivary action. A sustained release of the medicament is assured. Essentially, the method of preparation is the same as that for the moulded tablets. However, to make the lozenge more acceptable, it is usual to add flavourings or even colourings to the base.
Mix the medicaments intimately with the sucrose and acacia. Make the mixture into a paste with the water. Divide into 100 equal lozenges and dry. It will be apparent that if the medicament is in liquid or soft extract form, then a minimum of water will be required to form the cohesive mixture. The ideal consistency is that of bread dough, which may be rolled flat and the lozenges cut with a device similar to a pastry cutter, but of a smaller size. Such a device may be simply made with tin snips and pliers. Alternatively, the mass may be rolled into a pipe and suitably subdivided. |
Lozenges with a Flavoured Base. 11.39
Suitable flavouring bases which
will also lend colour, may be prepared from fruit juices free from preservatives
by reducing them to a soft
extract. Alternatively, use may
be made of essential oils or oleo resins. Remember that pharmacy is as much art
as it is science. Lozenges which are pleasant to the palate may be made from
essences or extracts of rose, violet, aniseed, liquorice or peppermint. These
are just a few of the possibilities open to a herbal pharmacist.
Simple Flavouring Syrup. 11.40
Heat 450ml of distilled water to boiling.
Add gradually, by stirring, 675g
of pure cane sugar. Continue
stirring over a low heat until all the sugar has dissolved. Filter, and then
adjust the syrup with distilled water to measure 1000 ml. The simple syrup may
be flavoured with essential oils or extracts. Ensure that such substances are
not antagonistic to any medicament which the syrup contains.
Elixirs (Elixeria) 11.41
The elixirs, as a Galenic
preparation, are aromatic, sweetened, spiritous liquids, which contain a
medicinal substance. As a pharmacy item, they are rarely encountered nowadays.
The popular recreational beverages known as Liqueurs, are in point of fact, the only commercial survivors of this true class of preparation, e.g., Chartreuse and Benedictine. These medieval Elixirs are usually of blunderbuss proportions. Due to the commercial value of such preparations, the recipes are closely guarded secrets. When a recipe contains a large number of medicinal plants, then it is inevitable that the question of incompatibilities and antagonists will arise.
The modern elixirs, as employed in pharmaceutical practice, are used purely as a flavoured vehicle to disguise the nauseous taste of a medicament. The following recipe is extracted from the United States Dispensatory, 21st Edition 1926. It will illustrate the principle.
Figure 11.41A

The Insufflation ( Snuff )
11.42
The origin of insufflation is to be found in Shamanic practice. The present
day South American shamanic cultures have an unusual delivery system which
consists of a long hollow tube. One end of which is a mouth piece and the other
in the shape of a small spoon in which a powdered plant drug is placed.
The crude drug is usually a mind altering substance. The shaman lies flat and the spoon end of the insufflator is introduced to his nostril. The acolyte then delivers the drug by blowing hard down the tube.
Tobacco snuff was fashionable until the late 1950,s. Snuff takers will attest to the speed and efficacy of this method of drug administration. Pharmaceutical practice makes use of a powder blower or insufflator to administer the powdered drug to the nasal passages. For best results, the drug must be reduced by trituration, so that it will pass a 60 or 80 mesh sieve.
The Inhalants 11.43
The use of steam, to introduce
volatile medicinal substances to the human system, is an ancient practice. We
normally associate that practice with the introduction of vapours to the nasal
or bronchial passages.
In some cultures the vapour is introduced to the mucous membrane by squatting over steam. Another method is by the use of sauna or sweat lodges. The medicament may be most conveniently used either as a solution such as a volatile oil introduced to hot water in a basin. The head and basin are covered by a towel and the rising vapours inhaled., alternatively, a 1:1 extract may be used at a ratio of 1ml to 100ml of hot water.
It is common to use a nebuliser that will reduce a solution to fine droplets for inhalation, either from a face mask or a tent. For self administration, a few drops of the medicament in a volatile form may be sprinkled onto a clean gauze pad. A more sophisticated commercial offering is the Nasal Inhaler, which is simply a wadded pad impregnated with a volatile medicament, which is contained in a tube for insertion into the nostril.
Homeopathic Preparations 11.44
There are 3 classes of
preparations for the administration of Homoeopathic drugs :
1. As the Mother Tincture and its attenuations.
2. Preparations of ointments and creams.
3. As the Triturations. This class may be administered either as a solution of the medicinal substance, or in tablets and pilules of various types, i.e., globules or granules.
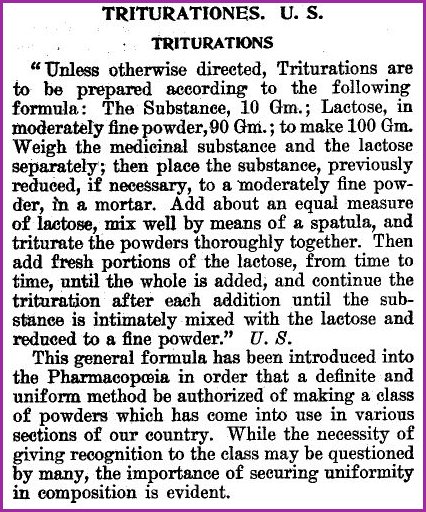
Triturations 11.45
Triturations were once official in the US Pharmacopeia.
The following figure is extracted from the
U.S. Dispensatory 21st Edition 1926.
Figure 11.45A
The Hahnemann Method. Organon 6th Edition
One-third
of one hundred grains sugar of milk is put in a glazed porcelain mortar, the
bottom dulled previously by rubbing it with fine, moist sand.
Upon this powder is put one grain of the powdered drug to be triturated. The sugar of milk used for dynamization must be of that special pure quality that is crystallized on strings and comes to us in the shape of long bars.
For a moment the medicines and powder are mixed with a porcelain spatula and triturated rather strongly, six to seven minutes, with the pestle rubbed dull, then the mass is scraped from the bottom of the mortar and from the pestle for three to four minutes, in order to make it homogeneous.
This is followed by triturating it in the same way 6 or 7 minutes without adding anything more and again scraping 3 or 4 minutes from what adhered to the mortar and pestle.
The second third of the sugar of milk is now added, mixed with the spatula and again triturated 6 or 7 minutes, followed by the scraping for 3 or 4 minutes and trituration without further addition for 6 or 7 minutes.
The last third of sugar of milk is then added, mixed with the spatula and triturated as before 6 or 7 minutes with most careful scraping together. The powder thus prepared is put in a vial, well corked, protected from direct sunlight to which the name of the substance and the designation of the first product marked /100 is given.
In order to raise this product to /10000, one grain of the powdered /100 is mixed with the third part of 100 grains of powdered sugar of milk and then proceed as before, but every third must be carefully triturated twice thoroughly each time for 6 or 7 minutes and scraped together 3 or 4 minutes before the second and last third of sugar of milk is added.
After each third, the same procedure is taken. When all is finished, the powder is put in a well corked vial and labeled /10000, i.e., (I), each grain containing 1/1,000,000 the original substance.
Accordingly, such a trituration of the three degrees requires six times six to seven minutes for triturating and six times 3 or 4 minutes for scraping, thus one hour for every degree.
After one hour such trituration of the first degree, each grain will contain 1/000; of the second 1/10,000; and in the third 1/1,000,000 of the drug used.
-::-::-
It will be understood from the description of the process, and the final
remarks in the US methodology
(Fig 11.45A) that a certain amount of friction existed between the
Allopathic and Homoeopathic schools. It will also be obvious that the Allopathic
school have not grasped the essentials of Homoepathy and the Hahnemann method.
Library
Pharmageddon
Herbal Block Index
![]()